Our Mission at Psychology Consultants
We can help you to
- Manage depression
- Cope with anxiety or stress
- Improve sleep
- Manage addictions
- Manage acute and chronic pain
- Management anger
- Adjust to personal loss or trauma
- Manage eating disorders
- Deal with child behavioural and emotional concerns such as anxiety and fear, sadness, and ADHD
- Improve parenting skills
- Cope with life transitions
- Make career decisions
- Enhance relationships
- Manage health concerns and
- Manage disabilities
Our Services
How we can help
Psychology Consultants has both male and female clinical psychologists and psychologists, each with broad experience in assessing, diagnosing, and treating people with a wide range of emotional and behavioural problems including anxiety and depression.
Our psychology services include
- Individual counselling – individuals, couples, and families;
- Group programs – Towards Better Sleep
- Careers counselling
- Workshops – Training Opportunities for Health Professionals (Motivational Interviewing with Dr Stan Steindl) Corporate Sleep Workshops with Kathryn Smith
Our Services

Brisbane Psychologists
Psychology Consultants has gathered together a professional team that is highly trained and very experienced. We have selected clinical psychologists and registered psychologists whose knowledge and skills are highly complementary of each other. Our goal is that our team’s wide range of professional interests and areas of expertise meet our clients’ diverse needs.
Latest News from Brisbane Psychology Consultants

You Hold the Key to Managing Change
By Ingrid Schults Change is necessary in all our lives. It is often a positive experience, but sometimes change is difficult to accept or to adapt to. MajoRead More
The truth about boredom
With Dr Alicia Carter Life is so busy that most of us would revel in the opportunity to feel bored but on the odd occasion that we or our children are bored,Read More

Top hacks to lessen Mother’s Guilt
So, how does society define a ‘good mother’? “Children don’t come with a manual and their wants and needs are individual. It is important to think about our Read More
How compassion can help people suffering from body weight shame
Tall or short, fat or thin, at the very core we all desire to be seen as attractive by those around us. Being seen as attractive in the eyes of another is keRead More
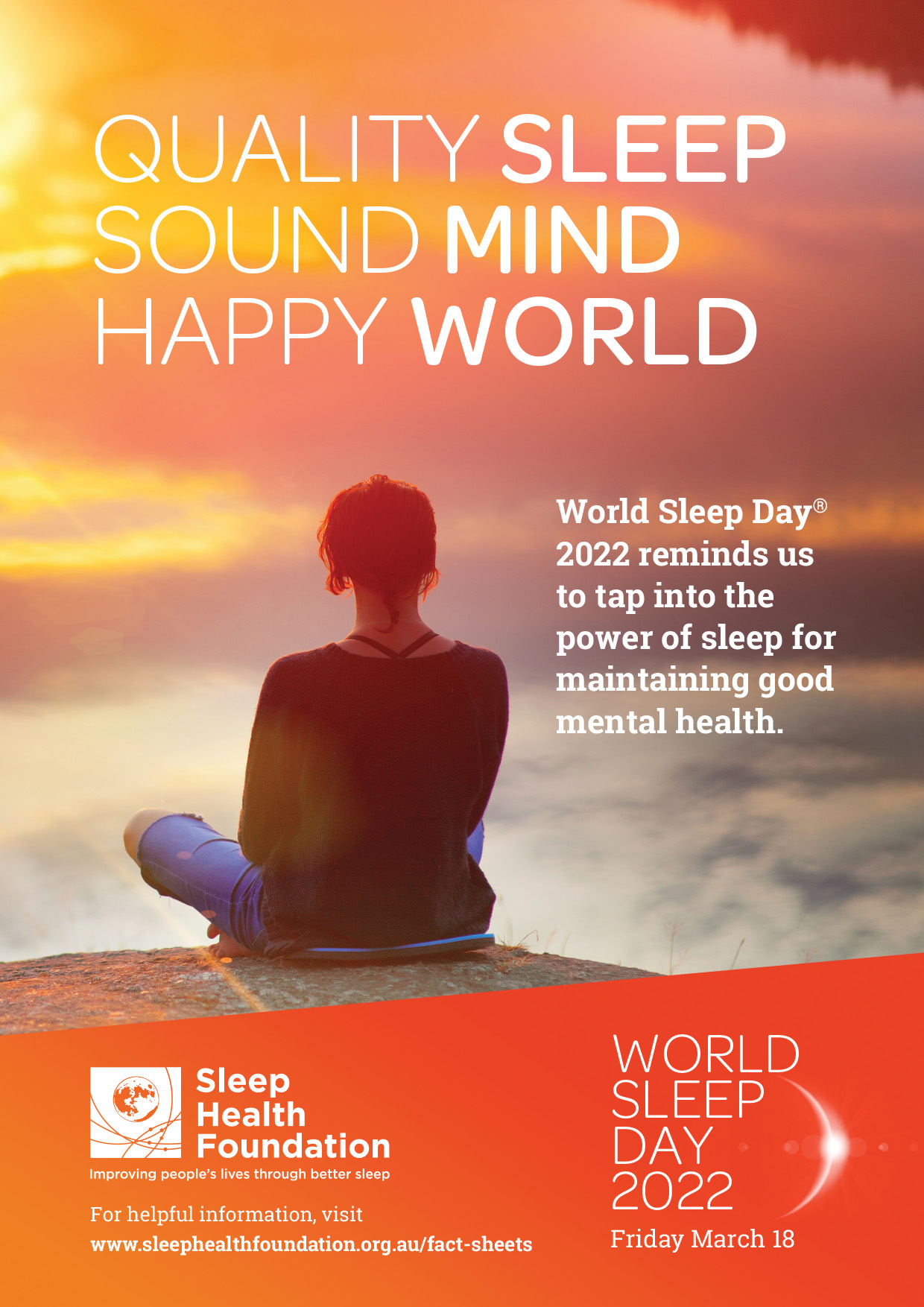
World Sleep Day 2022
Today is World Sleep Day! Does that mean we get to sleep all day? Well- actually that would not be good for us at all. World Sleep Day shines a light on the Read More

Riding the emotional rollercoaster of a health diagnosis
Interview with Psychologist Ingrid Schults 1.What are some of the common emotions felt by clients when diagnosed with an chronic illness? When anyone is diagRead More

Musing on 20 years of better sleep
“The biggest thing that most people worry about when they are not sleeping is not world affairs but simply about not sleeping!” Kathryn Smith There is a lot Read More

The power of positive psychology
Positive psychology is a growing, research-based field of study which extends beyond recovering from mental illness, to helping people thrive.
By focuRead More
Getting into the right head space
Reflect on a time when you weren’t in a good head space. Did your head feel scattered, were you frustrated, angry, anxious or just a bit sad? Now have a thinRead More

